12 Nov Lori and Taylor Linn
LORI
 I was diagnosed with Type 1 diabetes (T1D) a few weeks before I turned 10 years old. I cried when my mom told me. I imagine I was scared, but the only thought I actually remember was being upset because I thought it meant I could not go trick-or-treating and eat Halloween candy anymore. My dad also has Type 1 diabetes, so I had grown up around it. I think that had a lot to do with how they parented my diabetes as well. When I think about having no CGM and no pump, it amazes me that they let me be as independent as they did. As a parent now and knowing what I know, I’m sure inside they were scared, but they never let that show. They must’ve done a great job, because I don’t really have memories of T1D being a huge issue during my childhood. There were little things of course, I remember being awakened in the middle of the night for fingersticks (to test my blood glucose level), and I remember as a teen being embarrassed to tell people I had Type 1. Of course, back then carbohydrate counting wasn’t really a thing so eating sugary foods was definitely more restricted. My dad helped me navigate the T1D world and that was good. My mom was supportive as well; she was knowledgeable and participated in my care.
I was diagnosed with Type 1 diabetes (T1D) a few weeks before I turned 10 years old. I cried when my mom told me. I imagine I was scared, but the only thought I actually remember was being upset because I thought it meant I could not go trick-or-treating and eat Halloween candy anymore. My dad also has Type 1 diabetes, so I had grown up around it. I think that had a lot to do with how they parented my diabetes as well. When I think about having no CGM and no pump, it amazes me that they let me be as independent as they did. As a parent now and knowing what I know, I’m sure inside they were scared, but they never let that show. They must’ve done a great job, because I don’t really have memories of T1D being a huge issue during my childhood. There were little things of course, I remember being awakened in the middle of the night for fingersticks (to test my blood glucose level), and I remember as a teen being embarrassed to tell people I had Type 1. Of course, back then carbohydrate counting wasn’t really a thing so eating sugary foods was definitely more restricted. My dad helped me navigate the T1D world and that was good. My mom was supportive as well; she was knowledgeable and participated in my care.
It was comforting that my dad understood what I was going through: someone who has T1D “gets it” more. For many years, my dad and I made an afternoon of it going to our dilated-eye exam together (yeah, a T1Der’s eyes can be damaged by higher glucose levels, so we have to check them more frequently). It’s nice to have someone in your immediate family who understands life with T1D. We still frequently talk about our daily struggles, successes, lab work, tests and all that comes with Type 1 diabetes.
T1D’s biggest physical challenges for me were my pregnancies and always exercise. I like to work out, run, and strength train. Longer runs and workouts are difficult to maintain a balanced blood sugar level to avoid dangerous lows but without making my blood glucose too high at the beginning. It’s an ongoing battle. Pregnancies were challenging. I was incredibly committed to keeping my BG (blood glucose/sugar) numbers in target for the health of my babies. During all of my pregnancies I checked my blood sugar every 1 to 2 hours around the clock. It was exhausting, but worth it.
Emotional and psychological challenges? That’s a tough one. For me, the biggest emotional challenge is that no one who doesn’t have the disease can truly understand the all- encompassing effort it requires. From day today, minute to minute monitoring blood sugar levels, calculating carbs or even navigating the healthcare system to obtain the supplies we need to stay alive can be absolutely exhausting.
I get tired of people asking if there are certain things Taylor or I can or can’t eat, assuming we can’t have things because of T1D. I know it sounds superficial, and people are usually well-intentioned, but for some reason that gets to me. The bigger picture is the lack of education, awareness and knowledge about Type 1 diabetes. Working in healthcare, I am often blown away by even medical professionals’ lack of knowledge of Type 1 diabetes.
It’s also frustrating to hear people blame someone’s high and low blood sugar levels on the assumption that it must’ve been something he or she did wrong. That can be the case sometimes, but think about it: try managing anything perfectly 24/7/365. Type 1 diabetes is complex, its effects unpredictable and ever-changing, and we just try to get as much of it right as often as we can knowing we can’t do it perfectly like a normal pancreas can. It is an exhausting disease: I’ve said to my husband Joe that I’d just like to take off 24 hours from T1D. But that’s just not possible.
It’s hard to explain to people how many gray areas there are with T1D. As a friend once told me, managing diabetes is an art. That is so true. I think because so many things affect blood sugar levels in people with T1D and so many things in the body are affected by the disease, every instance and situation is never exactly the same twice in a row. Learning the nuances and developing the intuition on how to manage the disease just can’t be explained in a general way.
And hey, there are things I don’t want to hear! Please don’t tell me I “got diabetes because I eat too much sugar”, or ask me “why I have diabetes if I am not overweight!” We need to keep educating those around us about the difference between T1D and type 2 diabetes. That said, it’s important to help people understand that people with T1D can do anything anyone else can; we just have to prepare more and figure out how we’re going to manage our blood glucose levels while we’re doing it.
I also think it’s important for people who have T1D to have opportunities to connect with other people who have T1D. I remember when I was a child, the ADA (American Diabetes Association) had a monthly magazine with a penpal section. I reached out to several people, and ended up finding a lifelong friend with T1D who lives in Pennsylvania. Our parents let us get together to meet in person when we were teenagers, and we have seen each other several times since then. We have been there for each other through pre-teen and teenage years, marriages, births of our children, and many other life moments. I have another close friend who I met because of Type 1 diabetes: she and I both have T1D and each have a child with T1D. Having someone who understands in just so valuable.
Technology has come a long way, but there’s still no cure and T1D is still life-threatening. The tools help. I am currently on a closed-loop pump system with a continuous glucose monitor (CGM). I love it! I am very particular on how I manage my blood sugars, trying to keep myself in pretty tight range. This system allows me to keep more control, with the benefits of the CGM and closed loop. For many years I was in really good control being on insulin injections: I would take up to seven or eight injections a day. I was pretty hesitant to go on a pump, but I really liked my endocrinologist I had at the time and he strongly encouraged me to make the switch. Finally, I told him I would go on a pump, but only in preparation for trying to have our first child and then I’d go right back to injections. I remember him giving me a big smile, chuckling a little and saying he’d bet I would change my mind. My dad and I started on insulin pumps and went through the training at the same time, and I have never looked back. The CGM has been huge: knowing my blood sugar at all times is literally a dream come true! I remember as a child wishing for that. And now it is!
Thankfully my husband Joe does not have T1D. People with T1D are constantly running through all the calculations and symptoms in their head on how best to manage their T1D and most of the time we don’t verbalize it, so it can be hard for people to know how much work and effort we are actually putting in. I think for anyone living with someone with Type 1 diabetes understanding that it’s a constant is very important.
I only manage these things by the Grace of God! It can be very busy and tricky. I know everyone has things they balance in life, so this is no different. I have had T1D for over 30 years now, I have learned how to incorporate it into my everyday life. I don’t let it stop me from doing anything I want to do, whether it’s having children, running a half marathon, or having a big old ice cream sundae when I want to. I am very fortunate to have family and good friends who have and understand the disease and how it affects me. If I need to vent, if I have a question, I know I can reach out to them. Every single person has to figure out how to balance their health with all the other aspects of life. T1D is like that. I am very blessed to have such a full family and life.
Our son Taylor was diagnosed on July 13, 2021. I had seen the signs, and knew I was going to do a carb load and test him myself at home. To be honest, I just prayed that morning for the strength to get through whatever the outcome. Somehow when we got that “HIGH” reading on the glucose monitor I was able to keep calm, make the calls that needed to be made, and get him in for outpatient education. Looking back, the hardest parts of the day aside from obviously having to tell Taylor, was telling Joe and watching my oldest daughter breakdown and cry. She was 17 and her best friend since infancy has T1D…so she knew the challenges that were coming. My mom and nurse instincts kicked in and I just did what needed to be done. We have an incredibly supportive and knowledgeable pediatric endocrinology team. I was so thankful for them that day. They were so supportive and in the coming days and weeks were receptive to help get Taylor get on the CGM and pump as soon as possible, since we had the background and education to do so.
I am a pediatric and neonatal stepdown nurse, so I know there are many, many worse diagnoses that can happen to children. I certainly was not happy my child had T1D, but I also knew it was something we could handle. My good friend said that even though the above is true, I was allowed to feel sad and mad. Any feelings were okay.
 Honestly, while I knew we could handle Taylor’s diagnosis, it was hard for me to have people think this wasn’t a big deal, maybe because I try not to make a big deal of it myself. But having your child diagnosed with life-threatening disease that brings with it chronic, life-long implications is hard. It is life-changing. And to hear people say even with good intentions, “Well, at least you can help him”, doesn’t feel good. Yes, I can help him but that doesn’t mean it was easy for any of our family when he was diagnosed. Sometimes my heart does break for Taylor, knowing that this will be his life constantly from now on. Whenever my heart aches for Taylor, I then see how resilient and strong he is and how he’s rocking this T1D thing, and I feel better, have hope and am so proud of him.
Honestly, while I knew we could handle Taylor’s diagnosis, it was hard for me to have people think this wasn’t a big deal, maybe because I try not to make a big deal of it myself. But having your child diagnosed with life-threatening disease that brings with it chronic, life-long implications is hard. It is life-changing. And to hear people say even with good intentions, “Well, at least you can help him”, doesn’t feel good. Yes, I can help him but that doesn’t mean it was easy for any of our family when he was diagnosed. Sometimes my heart does break for Taylor, knowing that this will be his life constantly from now on. Whenever my heart aches for Taylor, I then see how resilient and strong he is and how he’s rocking this T1D thing, and I feel better, have hope and am so proud of him.
Taylor
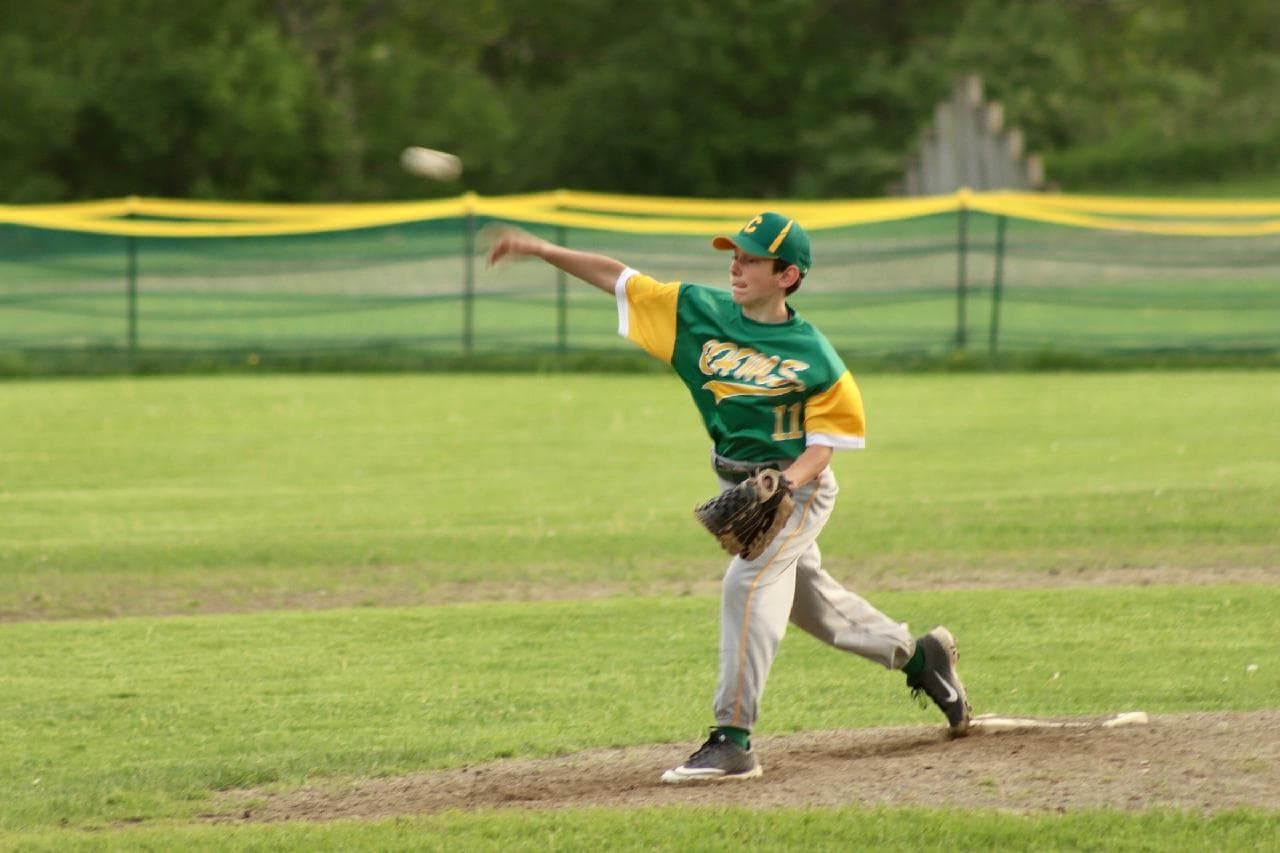
 Hi, I’m Taylor. I am 13. I was diagnosed with T1D last July. I love sports, and play baseball, basketball and football. Football is my favorite. The Green Bay Packers are my #1 team, but recently the Baltimore Ravens have become a close second. Last summer, my family and I had the opportunity to go to a Ravens training camp practice. One of their players, tight end Mark Andrews has T1D and wears the same glucose monitor as me. He and some of the players gave me a letter and some signed stuff. I like reading, drawing and watching movies. In the winter I like to play pond hockey with my family.
Hi, I’m Taylor. I am 13. I was diagnosed with T1D last July. I love sports, and play baseball, basketball and football. Football is my favorite. The Green Bay Packers are my #1 team, but recently the Baltimore Ravens have become a close second. Last summer, my family and I had the opportunity to go to a Ravens training camp practice. One of their players, tight end Mark Andrews has T1D and wears the same glucose monitor as me. He and some of the players gave me a letter and some signed stuff. I like reading, drawing and watching movies. In the winter I like to play pond hockey with my family.
I’m a 8th grader at Camels Hump Middle Scholl in Richmond Vermont. If I had to live with only one food, it would have to be Buffalo chicken pizza. My brother and I share a room together and while my mom wishes it was neater, it doesn’t look like a bomb went off in it. It doesn’t matter, we don’t spend a lot of time there.
OK, about my T1D. I don’t have any strong feelings on being diagnosed with Type 1 diabetes. I thought, “Okay, now I have this Type 1”, and I listened to everything everyone told me. Sports is where T1D has changed my life the most. Having T1D means I have to constantly pay attention to my blood sugar while I am playing sports. Starting an hour before I practice or play in games, I have to look at my blood sugar levels and insulin on board and determine a plan. That plan includes when/whether or not to take my pump off during the sports activity, and whether I need a snack before and/or during the practice or game.
Insertion sites (where I inject the canula for my insulin pump) bug me the most about T1D. They hurt going in, because it’s a big needle! And I have to change them every two days, sometimes even more often if a site does not seem to be working properly.
I think my friends understand most of it; a lot of them have relatives or someone else they know with T1D. I would like them to understand that even though I can still do all the same things, I just have to think and plan for how I will take care of my T1D while we do them.
It’s nice having my mom be a nurse and have T1D because she already knows all about it and she’s really helpful, like when she was able to advocate for me getting on a pump sooner! It makes things easier at school since she is the nurse there 3 days a week. My family’s also really good about my T1D.
If I could change one thing about managing my T1D, it would be that I wouldn’t have to change insertion sites or sensors-like I said, they hurt! It’d be great if they would just stay good forever!